Plugged Ducts & Mastitis
New evidence based guidelines about Plugged Ducts & Mastitis recently rocked the world of lactation. Let’s go over them and keep you up to date!
In 2022 the Academy of Breastfeeding Medicine (ABM) updated guidelines and released a new protocol titled “The Mastitis Spectrum”. You can find the new protocol in its entirety here. The internet still contains outdated and possibly damaging information. Staying up to date on new research can help your lactation journey immensely.
The Old Theory:
Previous information was based on the concept of “milk stasis” being the cause of mastitis and plugged ducts with common treatment methods being employed to “unplug trapped milk” including vigorous massage, frequent milk expression, fully emptying the breasts and applying heat. But we now know that “milk stasis” isn’t the problem and these solutions may in fact make the problem worse.
What is the Mastitis Spectrum?
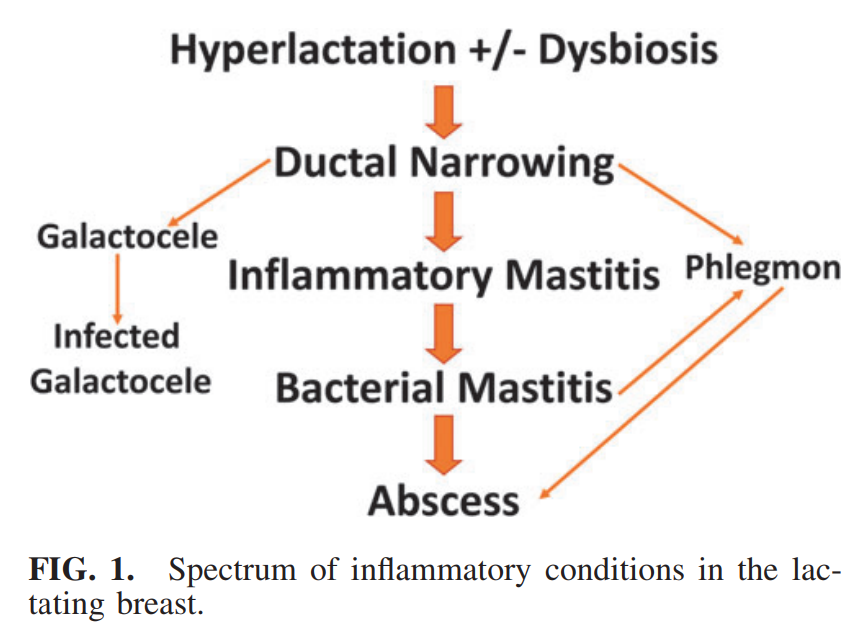
Mastitis is the name given to a range of conditions from “plugged ducts” to bacterial infection. Not every case of mastitis is the same and they don’t all require the use of antibiotics. The new ABM Protocol puts engorgement, plugged ducts, mastitis and abscesses all within the Mastitis Spectrum.
Figure 1 from Academy of Breastfeeding Medicine Protocol #36: The Mastitis Spectrum
The figure above shows the spectrum of mastitis with the underlying conditions being inflammation, often occurring within the context of Hyperlactation (too much milk) or Dysbiosis (disrupted microbiome).
Engorgement
Engorgement typically occurs between days 3-5 postpartum with the “milk coming in”. Symptoms of engorgement include breast/chest pain, firmness and swelling. Engorgement is similar to other conditions on The Mastitis Spectrum but is typically short-term relating to increased milk volume and swelling.
Ductal Narrowing & Plugged Ducts
Many people experience a discrete lump in the breast at some point during their lactation journey. It may feel tender, uncomfortable or painful. This can be referred to as a “plugged duct” but the name is misleading. It is rather Ductal Narrowing from surrounding breast swelling, lymphatic fluid congestion and dilated dilated capillaries. In other words, it’s not trapped milk, it’s inflammation!
Inflammatory Mastitis
Mastitis is an inflammation of the breast tissue that sometimes (but not always) results in an infection. Inflammatory Mastitis occurs when Ductal Narrowing worsens and the area becomes swollen, painful, warm and discolored. It may also come with other systemic symptoms like “feeling run down”, fever and chills. These symptoms are due to an inflammatory response but not necessarily due to infection.
Bacterial Mastitis
Bacterial Mastitis occurs when a bacterial organism disrupts the breast microbiome. It is not a contagious infection and it is safe to continue feeding the baby while treating bacterial mastitis.
Abscess
An Abscess may form if Bacterial Mastitis does not resolve with treatment. It is a well defined area of infected fluid and pus. Abscesses require medical treatment to drain the infected fluid.
Treatment for The Mastitis Spectrum
Imagine that you’ve sprained your ankle, how would you treat it? By resting it, using ice and taking anti-inflammatory medications. Many of the same principles apply for breast care within The Mastitis Spectrum.
Be gentle! Avoid vigorous and deep massage or use of vibration
Continue milk removal AS NORMAL. No need for extra pumping, feeding or “draining the breast”. Adding extra stimulation will increase supply (hyperlactation) and add more milk to the congested area. It will worsen the problem
Ice, Ice Baby! Apply ice after feeding or pumping for 10-15 minutes (use a cloth to prevent ice from being directly on the skin)
Use anti-inflammatory medications (NSAIDs) under the direction of your healthcare provider
Consider trying light lymphatic massage, this link is a video demonstrating the technique
Avoid saline or epsom salt soaks, castor oil rubs or other topical products on your nipples.
If the above treatment doesn’t alleviate symptoms within 24 hours or you have recurrent “plugged ducts”, reach out to an IBCLC and your healthcare provider. You don’t always need antibiotics but it may be a discussion to have.